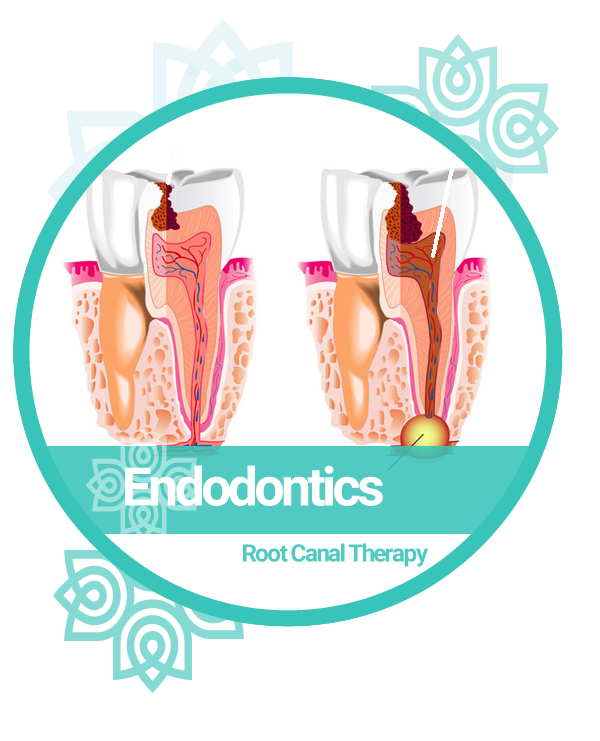
ENDODONTICS - ROOT CANAL THERAPY
ENDODONTIC THERAPY IS A SEQUENCE OF TREATMENT FOR THE PULP OF A TOOTH WHICH RESULTS IN THE ELIMINATION OF INFECTION AND PROTECTION OF THE DECONTAMINATED TOOTH FROM FUTURE MICROBIAL INVASION.
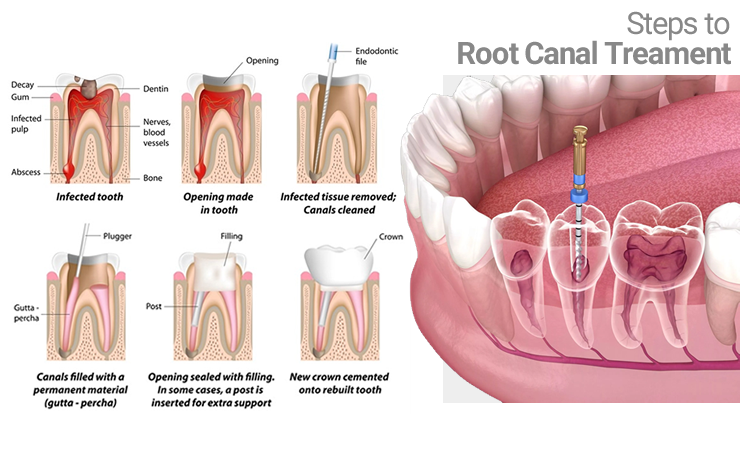
Root Canal therapy involves:
- the removal of these structures,
- the subsequent shaping, cleaning, and decontamination of the hollows with tiny files and irrigating solutions, and
- the obturation (filling) of the decontaminated canals with an inert filling such as gutta percha and typically a eugenol-based cement.
STEPS TO ROOT CANAL TREATMENT
| 1. Diagnosis of Periapical Infection | |
|---|---|
| 2. Accessing the Nerve Canals | |
| 3. Filing Canals and Irrigation | |
| 4. Sealing Canals with Gutta Percha | |
| 5. Build up and Post placement to Replace Missing Structures | |
| 6. Placing Crown to Protect the Tooth |
A tooth infection can lead to the formation of a fistula or periapical infection due to the spread of bacteria and inflammation from within the tooth to the surrounding tissues. Here's how this process typically occurs:
- Tooth Infection: A tooth infection, also known as a dental abscess, usually begins as a result of tooth decay, a cracked tooth, or a dental injury that allows bacteria to enter the innermost part of the tooth called the pulp chamber. The pulp contains nerves and blood vessels.
- Bacterial Proliferation: Once bacteria enter the pulp chamber, they can multiply rapidly, leading to infection and inflammation. As the infection progresses, it can cause intense pain, swelling, and pressure inside the tooth.
- Pressure Buildup: The infection and inflammation inside the tooth can cause pressure to build up. However, the tooth is enclosed within the hard enamel and dentin layers, which do not allow the pressure to escape easily.
- Fistula Formation: To relieve this pressure, the body’s natural defense mechanisms may create a pathway for the infection to escape. This often results in the formation of a fistula or gum boil. A fistula is a small tunnel-like tract that connects the infected area inside the tooth to the outside of the gum tissue. It acts as a drainage route for pus and infected material to escape from the tooth.
- Periapical Infection: As the infection progresses, it can extend beyond the tooth’s root tip (apex) and into the surrounding bone. This is known as a periapical infection. The periapical region is the area of bone surrounding the tooth’s root.
- Symptoms: The presence of a fistula or periapical infection may be accompanied by symptoms such as swelling, redness, tenderness or pain in the gum tissue, and the drainage of pus through the fistula. Patients often experience pain and discomfort that may radiate to other parts of the face.
- Dental Treatment: To address a tooth infection, a dentist or endodontist (a specialist in root canal treatments) typically performs a root canal procedure. During a root canal, the infected pulp tissue is removed from the tooth, the root canals are cleaned and disinfected, and the tooth is sealed. This helps eliminate the source of infection and pain.
- Resolution: After a successful root canal treatment, the fistula and periapical infection will generally heal as the infection is eliminated, and the body’s natural healing processes take over. Antibiotics may be prescribed in some cases to control the infection.